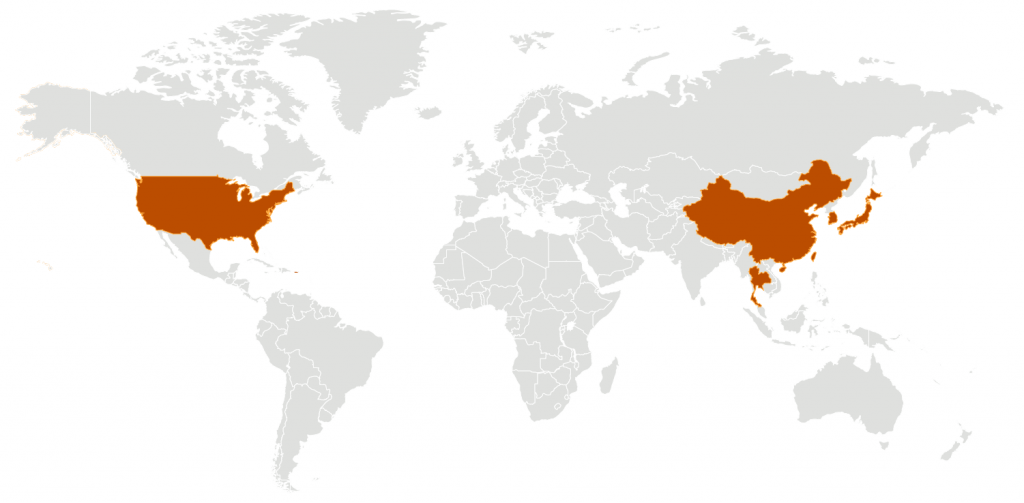
Ariel is Chinese American and a survivor of domestic violence — and the coronavirus pandemic has taken a painful toll on her mental health. It has created “a unique intersection in a time where racism against Chinese civilians is high, and domestic violence rates are increasing,” she tells InStyle.
Ariel, who was diagnosed with post-traumatic stress disorder (PTSD) three years ago, is one of many women across the country currently facing a resurgence of their symptoms. “I’ve relied on in-person interaction to fight off that anxiety,” she explains. “Now that we are under quarantine, my usual ways of fighting my trauma are gone. This is on top of the fact I am afraid of going out in public because I don’t want to be attacked.”
Like Ariel, anyone with previous trauma is at risk of being triggered by the pandemic. But it’s not only survivors that can experience PTSD symptoms during this time. Though we’re separated by physical distance, we’re all simultaneously absorbing the trauma of this unprecedented global event. Whether posted at home or working in the ICU, the threat of the virus and its impact on the economy are unavoidable weights to bear — and we’re all susceptible to long-term mental health issues like PTSD.
While no one experiences the disorder in exactly the same way, there are certain signs to look out for. “PTSD is a set of symptoms that result from trauma and can greatly impact functioning and create distress,” says Annie Miller, a psychotherapist in Washington D.C. These symptoms include: “anxiety, flashbacks, trouble sleeping, nightmares, lack of concentration, negative thoughts, and feeling easily startled.”
“People with PTSD often feel on edge and experience hypervigilance, which can cause irritability and an inability to relax, as well as a host of sleep problems,” adds Miller.
Allie, a social worker at a large outpatient dialysis clinic in New York City who works with infected patients, sadly knows these symptoms well. Last week her co-worker at another location in New York died from COVID-19, and she can’t help but wonder if she’ll be next. “I am a survivor of sexual assault,” she tells InStyle. “I am not new to PTSD, but this is a different type of trauma.” Being exposed to the virus, not to mention, the tragedies occurring daily in the NYC-area, is especially anxiety-inducing. “Not knowing if you’re going to die at 24 years old is worse than anything I’ve ever experienced in my life,” she adds. “How can you mentally prepare yourself for that?”
Allie believed that her PTSD was well-managed after working with a therapist, but the trauma she experiences now comes in a new form. “With my assault, I didn’t know [the attack] would happen. I had no idea. I didn’t wake up that morning knowing my life might get ruined. But with this, I wake up knowing what I’m doing could kill me and I have to tell myself ‘It’s OK,’” she says.
The coronavirus continues to remove any semblance of normalcy, leaving instead a scary, unsure world filled with mass graves, ventilator shortages, racist attacks, layoffs, and complete uncertainty of what will happen next. Though healthcare workers may be at a higher risk for developing PTSD during the pandemic, “people at home are also susceptible to the effects of trauma as we experience changes to our normal routine, job loss and fear about contracting the virus,” says Miller. “Worrying about loved ones getting sick and constant exposure to the news are also stressors that trigger the sympathetic, or ‘fight-or-flight,’ system in our brain. All of us have the potential to develop post-trauma symptoms.”R
Women at home are living in a state of “survival mode,” scared about which obstacle will be thrown at them next, what horrible reality they’ll have to digest, and unsure of what, if anything, they can do to prevent it. “Vicariously experiencing trauma and life-threatening situations can result in the development of PTSD,” explains Dr. Carla Marie Manly, a clinical psychologist in Sonoma County, Calif. “Those at home — like those on the front lines — may feel threatened by the coronavirus at every turn.” After a time, this heightened state of fear becomes the only way the brain can fathom moving through life.
Have you found that processing work, emotions, or even day-to-day tasks has become increasingly difficult as the pandemic has raged on? Or that you feel almost disassociated from your life? This may be a sign that you’re beginning to experience the effects of PTSD, often referred to as Pre-TSD. “Sleeplessness and lack of focus are frequently experienced,” explains Dr. Manly. “A general sense of depression or negativity can arise; some clients express feeling as if they are ‘in a fog’ or feel very numb. A general sense of dysphoria is very common.”
She continues, “Pre-TSD, which is not used as a clinical diagnosis, is often experienced as feeling ‘in overdrive,’ ‘very stressed,’ or ‘numbed-out.’ In this phase, some people note that they feel outside their own bodies. This is known as depersonalization. Derealization — the sense of being in a dreamlike or fantasy state — also often occurs.”
While anyone can be diagnosed with PTSD, women face a greater risk of developing the condition. According to the U.S. Department of Veteran Affairs, 10% of women in the U.S. will develop PTSD at some point in their lives, compared to just 4% of men. The National Alliance of Mental Illness (NAMI) reports that this is due, in part, to the fact that women as a group experience a higher number of traumatic events than men. In the U.S., 91% of sexual assault and rape victims are women, and 94% of women experience PTSD within two weeks of the incident. On top of that, one in four women experience domestic abuse in their lifetime.
It also tends to take women longer to get PTSD under control. The Office On Women’s Health reports that women have symptoms for an average of four years before diagnosis and treatment, compared to men, at just one year. (Though the reason for this difference is not reported, we surmise that the sexist habit in medicine of writing off women as “emotional” may have something to do with it). Women are also more likely to experience PTSD symptoms like anxiety and depression, or feelings of numbness, according to the Office On Women’s Health. One study from 2006 found that after 9/11, women reported feeling more panicked around the anniversary of the attack, and were more likely to re-experience trauma, compared to men.
A 2017 study says this difference is due to women’s “tend-and-befriend” response to traumatic situations, an alternative to the “fight-or-flight” response. Whereas men may come at trauma from a problem-solving mindset, women have been found to more often approach it at an emotional level. This begs the question, says Mary Joye, LMHC , if women are more likely to get PTSD because they typically fulfill the roles as nurturers in patriarchal societies, and become more emotionally invested in the problem. NAMI supports this idea, reporting that women in societies with more traditional gender roles experience PTSD at higher rates due to their high emotional vulnerability.
Before COVID-19, a reported one in four nurses was expected to develop PTSD in their lifetime. As healthcare workers (80% of whom are women, the CDC reports) show up day after day, often without proper personal protective equipment and supplies, those numbers may increase tremendously. “The hopelessness and not having treatment or a vaccine and seeing the repetition of cases is overwhelming,” Joye tells InStyle from her home in Winter Haven, Fla. “They are putting off the luxury of feeling their feelings when on this battlefield with an invisible enemy. They are taught to save lives and do no harm. Instead, they are losing lives, their colleagues are dying, and they have nothing to treat people with.”
Meghan, a nurse in Manhattan knows this well. “The chaos and the unknown rule the hospital units. We can’t process what is happening around us, nor do we have the time. After every shift I cry from exhaustion and frustration, I am broken from start to finish,” she says. “PPE carries an emotional weight and every time you put it on, it hits you like a wave. I will never be able to describe to you what it feels like to put it on everyday, the pain it causes from the breakdown on your face, the dirty overused mask and gowns, the armor for a battle we aren’t winning.”
Allie agrees. “I feel such an immense loss, to the point that I know that I’ve lost parts of myself to this that I’ll never get back. I feel anger, so much immense rage that I don’t even know what to do. I see [“re-open the economy”] protestors outside on Capitol Hill and I just want to scream at the top of my lungs,” she says. “I also feel so numb at the same time. Hearing again and again of folks that have passed.” Like most healthcare workers, Allie must remain isolated from her family and partner to protect them from potential infection, another toll on her mental health.
So, is there any way to cope? Dr. Manly stresses the importance of limiting exposure to negative news and seeking mental healthcare, if you’re able to, as soon as you recognize feeling traumatized or overwhelmed. While in-person appointments are currently unavailable, many mental health professionals are offering consultations and therapy remotely.m
Lisa*, an Emergency Room physician’s assistant, has tried using Headspace for Healthcare Workers, buying plants, using essential oils, FaceTiming with family, and sticking to her workout routine at home three to four days a week, no matter how tired she is. While some of these habits provide an in-the-moment distraction, the only true reprieve she’s found is the time at home with her daughter.
“Talking with friends and loved ones is also important, and a sense of being loved, safe, and supported can help reduce PTSD symptoms,” says Dr Manly.
The traumatic impact of the coronavirus will look different on everyone. If it leads to PTSD, that is nothing to be ashamed of. “Just because everyone else is dealing with the same trauma doesn’t mean we will all experience it the same way,” says Miller. “It is important not to dismiss symptoms that you notice and not to minimize what you are going through. Recognize that this is a traumatic experience and it is OK to ask for help.”
*Names have been changed.
The information in this story is accurate as of press time. However, as the situation surrounding COVID-19 continues to evolve, it’s possible that some data have changed since publication. While Health is trying to keep our stories as up-to-date as possible, we also encourage readers to stay informed on news and recommendations for their own communities by using the CDC, WHO, and their local public health department as resources
This Story Originally Appeared On instyle