Long-lasting insecticide-treated nets. Rapid diagnostic testing. Artemisinin-based combination therapies. None of these life-saving tools would have made it to market without the investment and engagement of the private sector and philanthropic foundations. It was through the wide-scale deployment of these and other tools that dramatic declines were achieved in the global malaria burden since the turn of the century. Bill Gates, Co-Chair of the Bill & Melinda Gates Foundation, offers a 360-degree view on why malaria is a top priority for his foundation.

In 2007, the Bill & Melinda Gates Foundation announced that malaria eradication was one of its goals, to “reach a day when no human being has malaria and no mosquito on earth is carrying it.” Why did the Foundation make the decision?
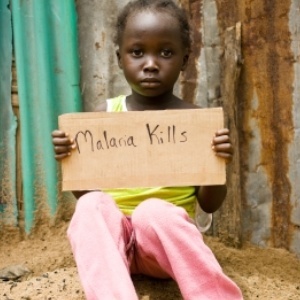
Malaria is a horrific disease. It’s one of the big killers of children, and it’s really holding Africa back because the healthcare and economic costs are incredibly large. When we picked health, particularly child health, as our priority, we knew we had to get engaged with malaria. Starting in the year 2000, it was a priority for us. The Global Fund came together a few years later, and then, at the 2007 meeting, we articulated the idea that if we orchestrated enough innovation, we should be able to shrink the malaria map and, eventually, bring it to an end.
How well do you feel we are all doing in reaching this goal, 11 years on?
One of the key metrics, probably the most important metric, is cutting down the number of deaths due to malaria, and if you take the last decade, we’ve done very well. But as usual with malaria, if you stand still, both the mosquito and the parasite itself evolve around your tools; the insecticides for the bed nets and the spraying in the case of mosquitos, and the drugs in the case of the parasite itself. In the last few years, we have seen an increase in cases, which means we’ve got to get this pipeline of new tools out there and deployed.
The tools are one side, but there’s also the political aspect. We need to invest in research and development, but one of the other challenges has been a plateauing in investment.
We’ll do our best to get increased investment, but it won’t be a dramatic increase. We have to take the dollars we have and gather data about where we can amplify its impact. The donor countries have been generous, and it’s great the United Kingdom renewed its commitment, and our Foundation committed an additional US$ 1 billion to the fight. So, we’re getting smarter all the time, and it’s great that the donors have stayed with this fight, particularly the Global Fund who has been the biggest buyer of the bed nets and the spraying ingredients.
What arguments do you use when you’re trying to convince others to get on board, whether it’s a funder or a politician?
If they have malaria in their countries, and you saw your neighbour suffering, the response would be quite phenomenal. Here, the challenge is that most people don’t get to go to Africa and see what it’s like in the Democratic Republic of Congo or Nigeria, or the regions that still have extreme numbers of cases. So using the latest communications tools to show them what that burden looks like, explaining how we’re driving the price of all of the tools down, and getting smarter about getting them to the right places, they should share in this excitement that deaths are down very dramatically. We’re adopting at this London summit a very aggressive goal: that if all the partners come together, we should be able to cut malaria cases in half again by 2023.
What are some of the malaria-fighting tools that we see in the pipeline that you are investing in that you think will be useful?
The 3 key tools right now are the insecticide we use for the spaying, indoor spraying, and there’s a good pipeline there with the Liverpool-based IVCC, the Innovative Vector Control Consortium, working with the chemical companies; the insecticide we use on the nets themselves; and the drugs – we’re refining which artemisinin combinations are most effective. There’s been good progress and there are some new drugs in the pipeline for P. vivax. GSK is very close to getting Tafenoquine out and available, so that’s going to be a great tool; and then, we have a new generation of diagnostics that are somewhat more sensitive.
We’ve got the idea of a second-generation vaccine that would have enough duration to be a very powerful tool. And finally, there’s work in the laboratory on mosquito genetics, and how using CRISPR-related tools, we might be able to, at least temporarily, cut mosquito populations, which would help us a lot to clear areas and reduce the malaria map.
Out of all these topics, which ones do you get most excited about?
The Foundation is a big funder in the R&D space, actually the single-biggest funder, so we have product development groups like Medicines for Malaria Venture (MMV) for the drugs, Malaria Vaccine Initiative (MVI) for the vaccine, so I think they’re all very critical. I also like the modelling work that we’re doing that helps understand which tools are most important in which areas. If you have the indoor biting, then the nets and the spraying are super-effective; if it’s more outdoor biting, then things like these attractive sugar bait traps that are coming along may be the most important tool.
The gene drive, or gene editing, is kind of the new kid on the block. It’s not fully figured out exactly what the profile will look like and what the regulatory pathway is, so we’re not counting on that, but particularly as we move into the toughest areas, where the biting rates are very high, it’s clear that would make a huge difference if we could get it.
It’s interesting because it sounds like there are the high-tech tools and the low-tech tools. You may have data that shows you the need for using two insecticides in your bed nets, but in the end, you’re still talking about parents making sure that they have a bed net and that their whole family is sleeping under them. Tell me a little bit about the work in communities and what can be done to make sure those tools are being used better.
You’re absolutely right. On-the-ground coverage is key to this, even things like case tracking, where you get the cases reported and then you’re able to go to the family and neighbours of those people and try to make sure that it’s not spreading further. The message on bed nets: When we first bring them out, we get good compliance but then, over time, when we’re not keeping that message fresh, we see not only that people stop using them, but eventually they deteriorate physically. We’re really looking at that durability issue.
We’re also looking at which community groups are trusted to get the message out. We have African leaders coming together under the African Leaders Malaria Alliance (ALMA), a group that provides data about which countries have done the best job getting the message out and try and spread best practices. African leaders have been a big part of this, and they understand how to activate those local communities, so we need them and that’s been critical.

